 In late August, Anthem announced it will no longer cover CT scans and MRI performed in hospital outpatient departments unless deemed medically necessary. To receive payments from Anthem, imaging tests are subject to preapproval to confirm they’re medically necessary*.
In late August, Anthem announced it will no longer cover CT scans and MRI performed in hospital outpatient departments unless deemed medically necessary. To receive payments from Anthem, imaging tests are subject to preapproval to confirm they’re medically necessary*.
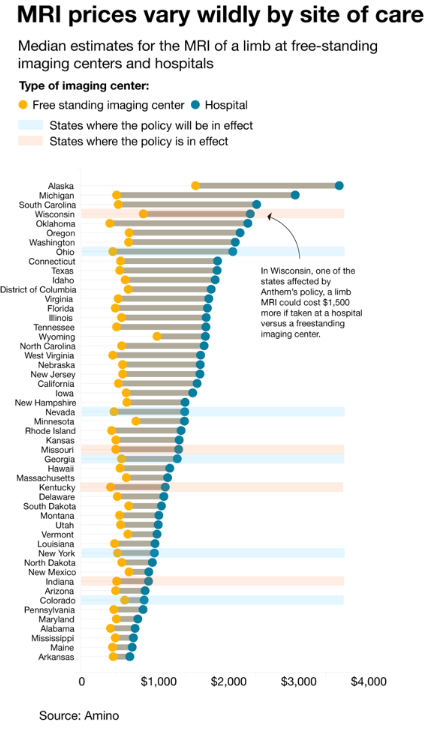
This policy has been in effect since July 1 in Indiana, Wisconsin, Missouri, and Kentucky, with expansion into Ohio, Colorado, Georgia, Nevada, and New York on September 1. A total of 13 states are expected to be under the policy by March 2018 (New Hampshire has been exempted from the program for the time being). The policy is intended to direct services to lower-cost freestanding imaging centers. Under the policy physicians ordering a test will be provided a list of centers eligible for patient referrals.
While this policy may come as a shock to some, in 2013, Anthem launched the Imaging Quality & Cost Program in Kentucky to provide patients with information regarding how facilities compared in terms of quality and cost. This move was intended to empower members to make informed decisions about healthcare. Anthem members who had been pre-approved for imaging were directly contacted by an Anthem outreach specialist and provided information about alternative locations with high-quality imaging providers that were lower cost.
The new policy is in line with the overall trend toward value care – high quality at lower cost. It is also in line with the newer aggressive approaches we have seen on the government payor side regarding MACRA. Anthem encouraged a lower-cost alternative for several years and now is forcing the issue. Data show that costs of care are lower in the free-standing locations, and in some states to a shocking magnitude.
According to outcry from the American College of Radiology, this policy undercuts the physician-patient relationship. The policy would punish rural and inner-city patients disproportionately, as the local hospital outpatient setting may be the only immediate access point for advanced imaging outside of the main hospital. While areas that do not have a freestanding imaging center, such as rural locations, will likely be covered under medical necessity, there is concern regarding retroactive lookback at imaging services provided in the emergency department and payment denial if the situation is determined to be not truly related to an emergency.
This policy lends itself to the overall discussion we have been having at Stroudwater about assisting clients in right-sizing their services and footprint. As we push hospitals to diversify their portfolios and examine their outpatient services from a cost-of-care perspective rather than enhanced HOPD reimbursement, this change in policy is at the forefront of discussions with clients in affected states.
Stroudwater provides a full-service ambulatory development plan that begins with overall strategy for a system and addresses the market needs, service complement, physician strategy and facility design necessary to execute the ambulatory development.
*Medically Necessary:
An advanced radiologic imaging procedure in the hospital outpatient department is considered medically necessary when any of the following are present:
The services being provided are only available in the hospital setting; or
The individual requires an obstetrical observation; or
The individual is receiving perinatology services; or
There are no other geographically accessible appropriate alternative sites for the individual to undergo the procedure, including but not limited to the following:
Moderate or deep sedation or general anesthesia is required for the procedure and a freestanding facility providing such sedation is not available; or
The equipment for the size of the individual (that is, very small or very large) is not available in a freestanding facility; or
The individual has a documented diagnosis of claustrophobia requiring open magnetic resonance imaging which is not available in a freestanding facility.
Not Medically Necessary:
All other advanced radiologic imaging procedures in the hospital outpatient department are considered not medically necessary when the above criteria are not met.
Sources (not exhaustive):
https://www.anthem.com/medicalpolicies/guidelines/gl_pw_c191757.htm
http://www.modernhealthcare.com/article/20170826/NEWS/170829906
