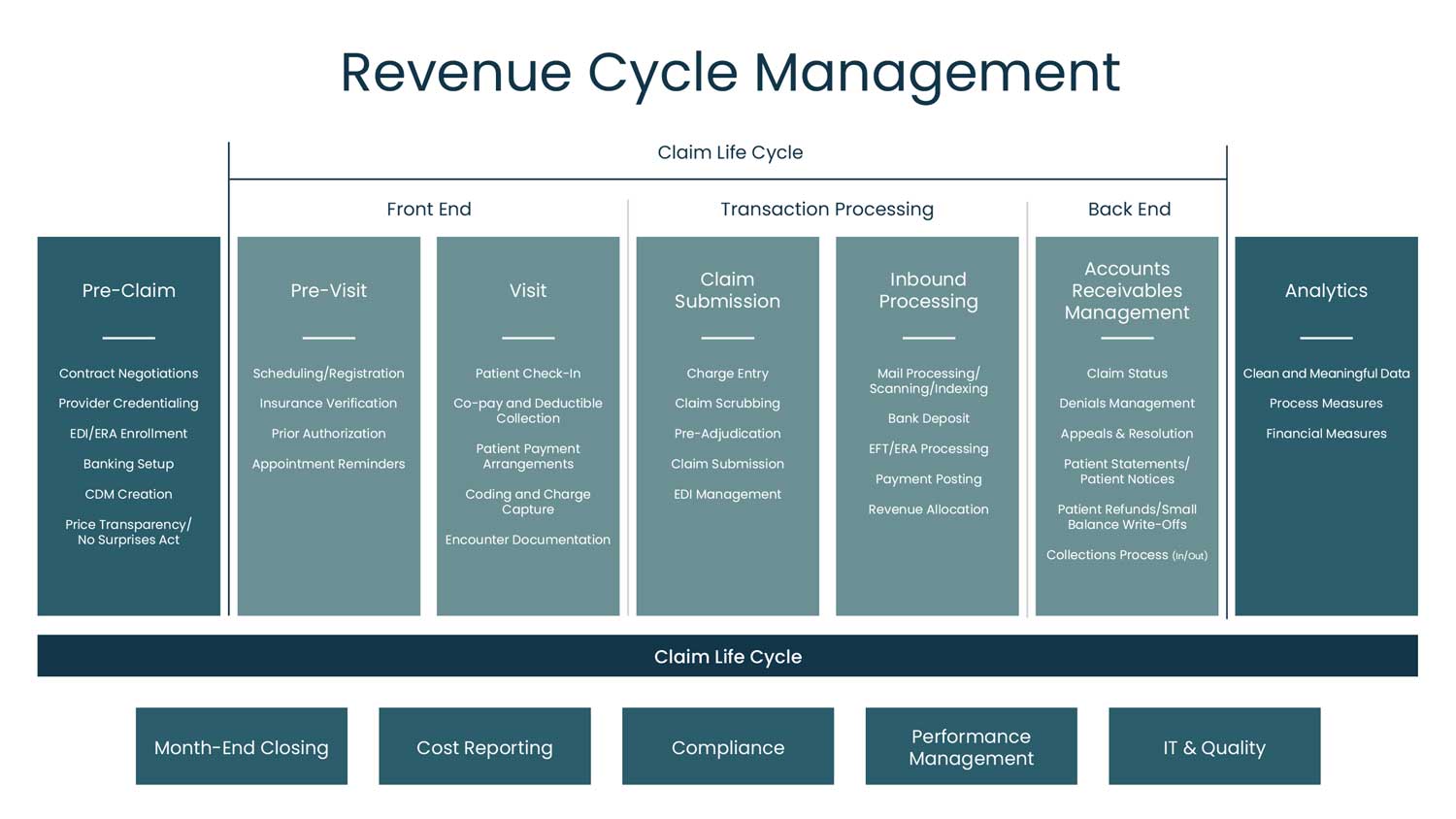
For healthcare providers and organizations, revenue cycle management activities are multifaceted and take place in several distinct stages. While many might see revenue cycle activities as beginning when the patient arrives for a visit, the foundational activities of revenue cycle management truly begin long before the appointment time. These include pre-claim, non-patient-facing activities such as contract negotiations, provider credentialing, and price transparency.
Improving the hospital’s revenue cycle processes at each stage will contribute to the long-term financial success of the provider organization. The following are a few important steps Critical Access Hospitals (CAHs) can take to improve efficiency in pre-claim activities and overall revenue cycle management.
Payer Contract Negotiations
Collect and review all current contracts:
- Do you have copies of all of the agreements, including all amendments and the most current fee schedule?
- When was the last time that they were signed?
- Does your team know what you should be collecting?
Pay careful attention to special clauses that can affect payment. Is your team aware of the “lesser of” clauses, where the payer will pay you the lesser of their fee schedule or the charge amount? If your hospital’s prices are set below Medicare, you may be leaving money on the table. How does your contract address timely filing windows? Does your team have updated information on timely filing deadlines and payment windows? You should ensure that your contract provides for enough time to correct/refile or appeal erroneous claims within these set timeframes.
When reviewing the contract, you will want to conduct modeling to project the impact of the contract on your hospital’s bottom line. Look closely at the reimbursement methodology language included in payer contracts, such as:
- Excluded services that should not be priced for that payer (COVID-19 testing, for example, was not included in anyone’s contract in 2020 but quickly became relevant)
- Fee schedules that are fixed to a point in time
- Clauses that limit the annual increase percentages
When renegotiating existing contracts, look for ways to voluntarily reduce your overall charges to get a higher percentage of charge reimbursement.
Provider Credentialing & EDI Enrollment
The credentialing and enrollment process for newly hired providers is notoriously complex. Examine your internal process and the people involved in each step:
- When a new provider is hired, how many different people are they in contact with?
- Who is gathering all of their information to credential them in the hospital?
- How is that information passed along to the revenue cycle team who will enroll them with payers?
- What is the banking set up for the provider? Where will their payments go?
Chargemaster
The chargemaster (CDM) is made up of three key elements:
- Price: The charge for the procedure
- Revenue code: Where the services were provided
- CPT/HCPCS Codes: The services provided, translated into codes used for billing
Look at these four key areas to adopt chargemaster best practices:
- Missing CPT/HCPCS Codes
CDM records where no CPT/HCPCS codes are listed
- Invalid CPT/HCPCS Codes
CDM records where CPT/HCPCS codes are not listed on AMA or CMS data files
- Below Medicare Fee Schedule
Price assigned to CPT/HCPCS codes is below the CMS fee schedule
- Same CPT/HCPCS, multiple prices
A different price is assigned to the same CPT/HCPCS code
Ask the following questions:
- Does your hospital have a strategy established for pricing? Is this strategy defensible?
- When was the last time your entire hospital chargemaster was reviewed?
- Is pricing consistent?
- Do you have a policy for ongoing CDM maintenance?
Price Transparency
CMS requires you to review price transparency in your shoppable services annually. Your hospital’s revenue cycle team will need to review the information presented every year and update any changes in standard rates, negotiated charges, ancillary services (new or revised), and the 300 listed shoppable services noting new and deleted services. Be sure the document you publish has a date on it so anyone reviewing the document will know it has been reviewed within the past 12 months.
In Closing
Revenue cycle activities are complex, multifaceted, and interdependent, and take place at each stage of a patient’s journey through the healthcare system. A positive or negative change in one area, like CDM pricing or shoppable services, can affect others such as cost reporting and payer contracts. Keep in mind that when one area of revenue cycle management runs smoothly, it has a domino effect on all other processes in the system, improving outcomes for both the patient’s experience and the hospital’s bottom line.
Contact Stroudwater to learn more about improving your revenue cycle management.
