Nurse leaders from Cox Monett and Cox Barton Critical Access Hospitals shared their experience in developing a successful swing bed committee within the Cox Health System (Missouri).
This session explored how collaboration, data analytics, and operational efficiencies have led to swing bed volume growth, improved patient care, and enhanced program performance.
Attendees also gained actionable insights into using the Stroudwater Swing Bed Quality Reporting Program to expand and optimize their own swing bed services.
Key learnings include:
- Develop a Swing Bed Committee for Growth – Understand the process of establishing a swing bed committee within a hospital or health system to improve capacity and coordination.
- Utilize Data to Drive Quality and Outcomes – Learn how to leverage data analytics and performance tracking through the Stroudwater Swing Bed Quality Reporting Program to improve swing bed program quality and patient outcomes.
- Enhance Communication and Coordination – Apply lessons learned from real-world case studies to strengthen collaboration across healthcare organizations and drive sustainable swing bed program growth.
Q&A
Unfortunately, I do not have a good way to run a report for ADC, but we have estimated that at Monett’s average would be 3-4 every day. Currently we have 8 on our unit and have been up as high at 10.
On our 2024 DNV survey we had corrective action plans related to vision and dental needs: How do we know that our patients have vision and dental needs if we do not assess them in those areas. We added a requirement for swing bed patients to have a vision and dental assessment completed upon Swing Bed Admission. For the nursing team to remember, we created an electronic “nursing task communication” to complete the vison and dental assessment. We’re also incorporating in our new Epic record.
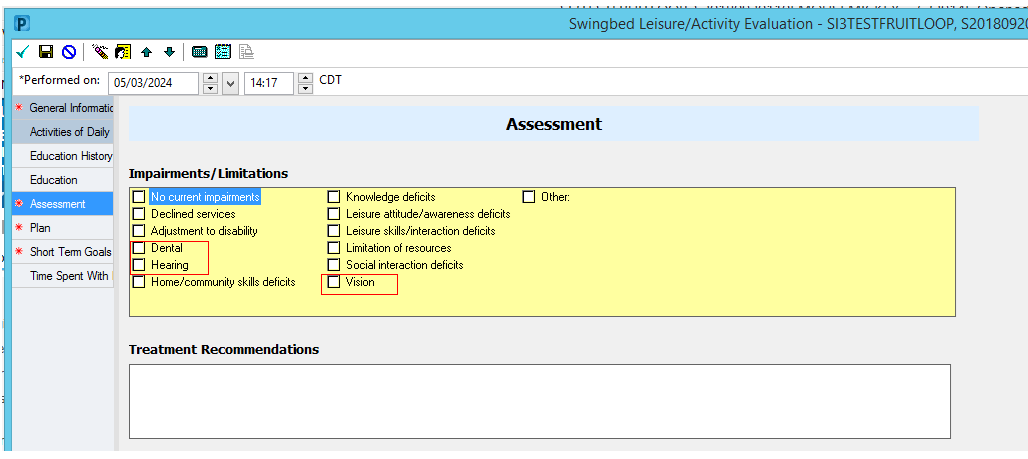
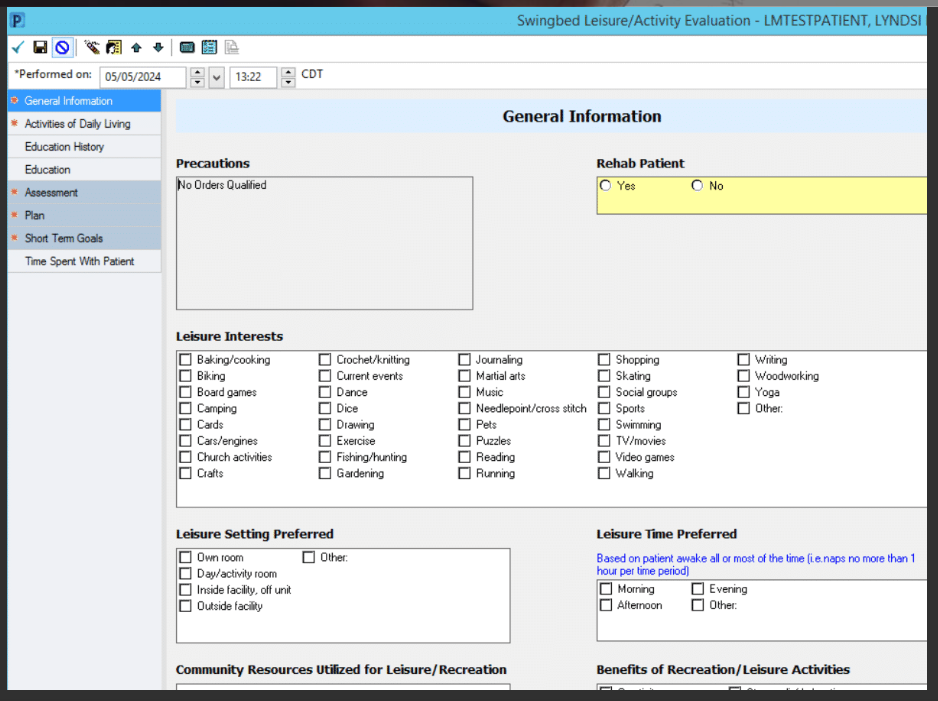
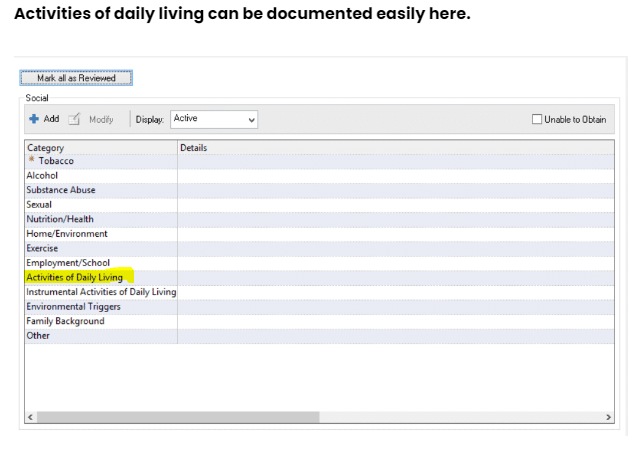
In addition, we received another non-conformity related to their Customary Routine. For example, what does their typical day look like at home when they are feeling well and following a routine. We created a documentation field in which we named “Swingbed Leisure/Activity Evaluation.” This is meant to capture hobbies, interests, and ADL routines- including when they like to do specific activities and tasks. This survey year they focused more on when they like to eat and shower.
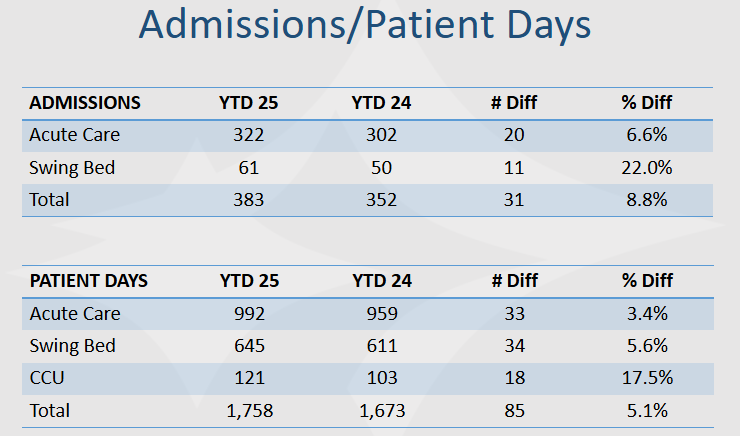
We have seen our Medicare and Medicare Advantage payor mix creep up slightly year over year, but this has remained steady, and we did not see a large increase outside of years past. Our ALOS for Med Surg was 3.13 and our Swing Bed was 8.41.
This has been a focus for us, and we recognize that we are still not where we wish to be. Our goal if from receiving a referral to acceptance of 4 hours or less. As soon as the referral is received, we send it on to the team (Therapy, Nutrition, Pharmacy, Nursing, and sometimes the provider if nursing feels there is medical clearance needed). It takes a lot of teamwork and buy-in of the staff to understand the importance of a quick reply. At Barton, their House Supervisor reviews referrals if they come in on weekends and evenings, and Monett would like to see what we can do to offer greater coverage 7 days a week.
We do not have it on an order sheet, but it is reviewed and discussed during morning huddle with a focus on day 2. Our NM/ANM and now coordinator are proactive and many times will have already identified who they wish to start approval on prior to day 2.
We start early on advantage plans (even from day one) if we feel they are going to be a candidate for Swing Bed. We try to have thorough and supportive documentation to show the need and then make frequent follow-up calls. We have missed out on a couple because we could not get the acceptance back prior to discharge.
Back story: Our Activities Coordinator has previous training in OT, but did not pass her licensure examination. She went through our Unlicensed Assistive Personnel training which allowed her to sit for the Certified Nursing Assistant exam.
Duties: She works very closely with our therapy department. She assists patients with ADLs. She attends the daily 10:00 Multi-D huddle (Pharmacy, Nursing, Providers, Case Management, Therapy, RT). She does document on the progress of the patient on items that are within her scope of practice. She organizes group activities (Bingo, music, prayer, crafts, etc.). She also visits the patient and if part of their routine is manicure, hair dressing etc. she will do their hair and nails. She does the 30 day post DC follow up phone calls on SB patients and enters our Stroudwater data.
For Monett our UR nurse was also our Swing Bed coordinator. Upon her retirement our system has taken over our UR duties remotely from Springfield and allowed this position to now be solely focused on the Swing Bed program. So overall the employee count did not change for us, just a shift in duties. For Barton this will be a completely new position, and we will track to see if their growth going forward will offset the salary of the coordinator.
For Monett we are 8.5 days. This is the lowest in the state and also nationally. The committee is doing a deep dive on this to assure that we are not having any type of adverse impact by the shorter stay.
At Barton, we average about 11.7.
